Specialist Capacity Challenges
How can a health system handle new high-value referrals when their specialist providers are at capacity?
Let's talk about specialist referral capacity constraints. One of the most common questions we get at Care Continuity is "how can a health system handle new high-value referrals when their specialist providers are at capacity?" Care Continuity can uncover new specialist referral opportunities coming from ED discharges, for example, but if specialist appointment schedules are already full, how can that clinic accommodate any additional referrals and grow procedure revenue for the health system?
Understanding the appointment capacity challenge
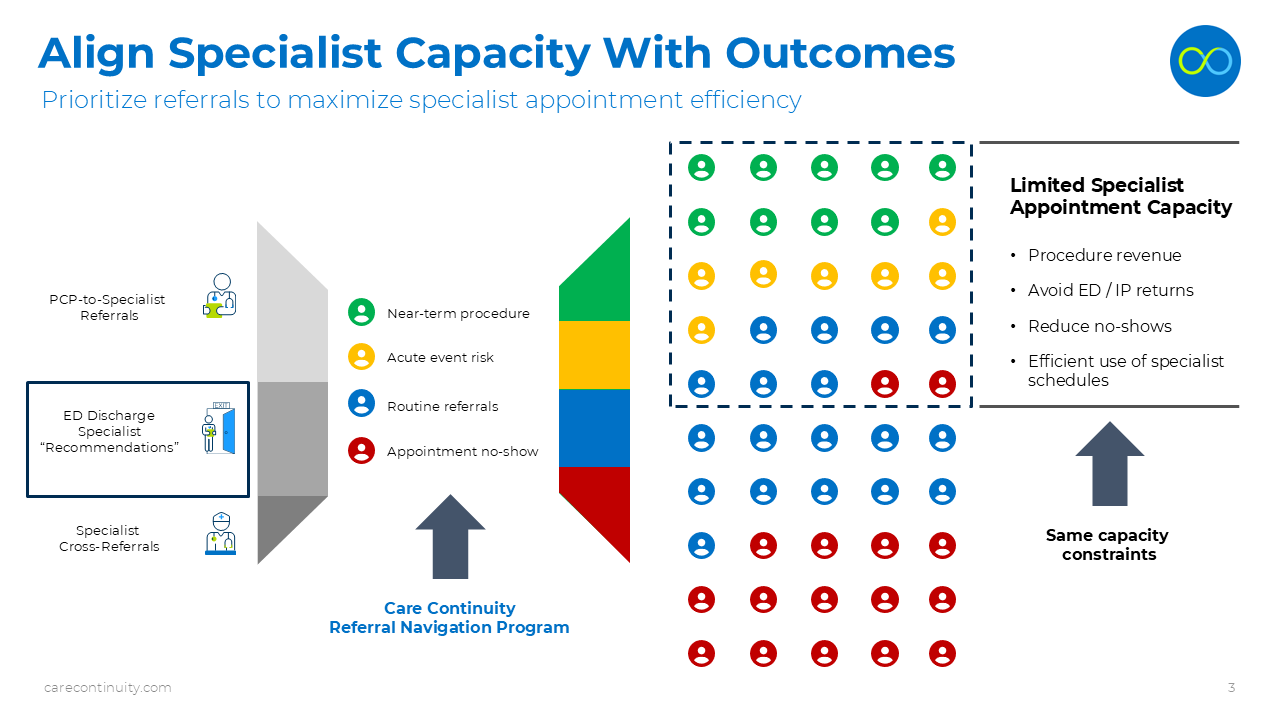
Despite having limited appointment capacity in many specialist offices, health systems often struggle to prioritize the highest impact referrals. Not all specialist referrals are equal, and despite 90% of referrals being submitted as “routine”, each of these patients can have very different expected outcomes and behavior. Some patients will require near-term procedures that drive downstream revenue for the health system. Other patients are high-risk from a clinical perspective and could wind up with an unplanned acute event. Many of these referrals lead to scheduled appointments, but the patient is non-compliant and doesn't show up. Even with a centralized approach, the referral scheduling process is typically first in, first-out, meaning the prioritization is based on referral date, not expected outcome.
The result is a random mix of patient referrals, and an inefficient process to predict the highest-impact appointments that will drive outcomes for the health system. This diagram shows the sources of specialist referrals on the left, the potential outcomes for each patient in the middle, and the dotted lines on the right represent the limited appointment capacity of specialist offices. With no meaningful prioritization of routine referrals, these specialists are not using their time efficiently - missing high value and high risk patients that should be at the top of the referral pool.
A smarter approach to referral prioritization
Now let’s look at how the Care Continuity Referral Navigation program applied a smarter approach to prioritizing referrals to ensure that limited specialist capacity is used most efficiently. By applying predictive modeling and analytics, Care Continuity can understand the expected outcomes for each patient in advance, re-prioritizing the pool of referrals so that the right patients fit inside that limited capacity box. Even with no additional appointment capacity, a specialist provider now captures all of the likely downstream procedures (in green), and high-risk patients (in yellow). While shifting more routine referrals and likely no-shows to better suited provider resources like an APP or PCP. The same appointment capacity, but a smarter use of specialist capacity, aligned with better outcomes. Furthermore, this diagram also shows the impact of high-value referrals found in emergency department discharges. Many patients leave the ED with a specialist follow-up recommendation, but few of them are prioritized for appointment scheduling or navigation. This is another way that Care Continuity improves the mix of specialist referrals, by uncovering daily ED discharges that require near-term downstream procedures, adding these patients to the referral pool and prioritizing them for specialist appointments. Further improves this smart stratification approach.
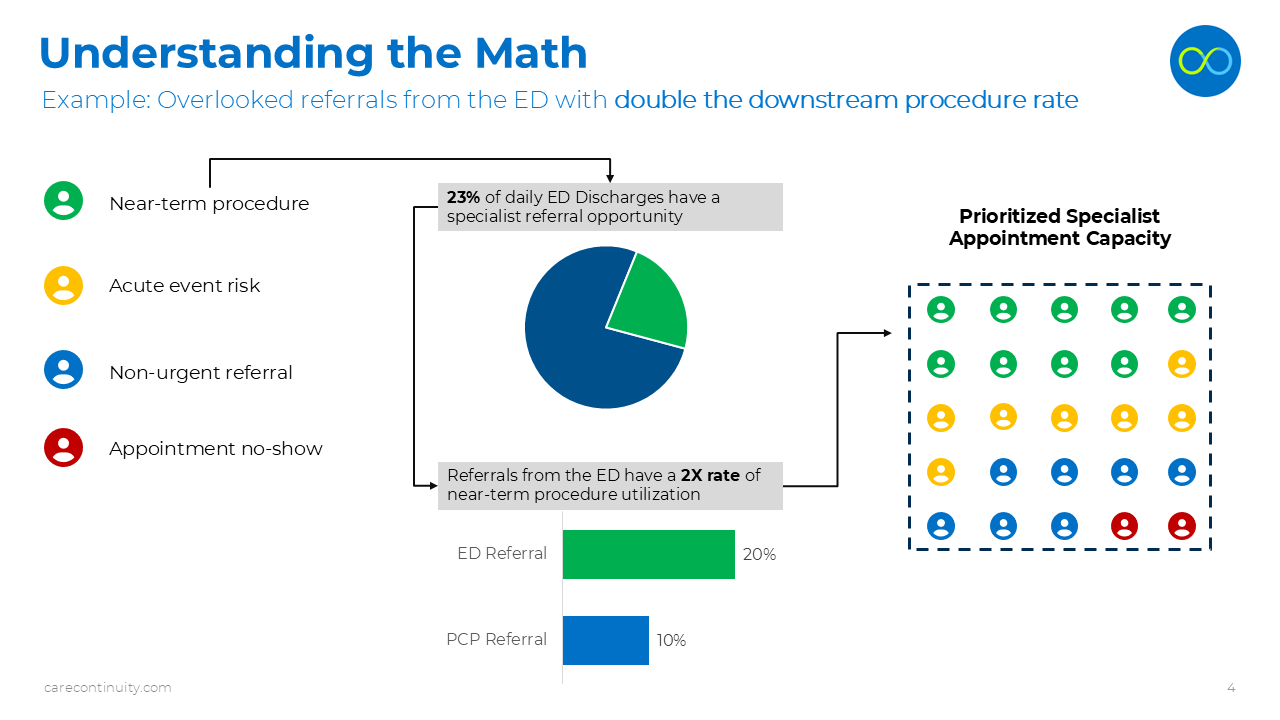
The Value Equation
Here’s the basic math, using an example of referral opportunities among recent ED discharges. Most health systems are not actively navigating these ED patients once they leave, although many have important specialist follow-up recommendations. This is a valuable source of new referrals - in fact Care Continuity sees that about 23% of daily ED discharges actually have a specialist "recommendation" buried in the ED provider notes. In addition, these patients that entered the health system through the ED, have a significantly higher rate of requiring near-term downstream procedures. While the general population of PCP-to-specialist referrals has about a 10% rate of downstream procedure utilization, ED referrals are typically double that at20%. The math is simple - getting more of these valuable ED discharges into the specialist referral pool and prioritized for limited appointment spots, has a significant impact on specialist provider efficiency and downstream revenue opportunity. Again - using the existing appointment capacity, specialist offices can prioritize the right patients to drive downstream utilization and avoid valuable procedure leakage.
A simple summary of our answer
In summary, limited specialist appointment capacity is a challenge for every integrated health system and medical group. Given this constraint, the Care Continuity solution is all about using existing capacity more efficiently, and building a smarter program that aligns specialist referrals with desired outcomes. By better matching appointment capacity with the right patients, health systems can support more efficient operations for their medical group offices, while also driving incremental revenue for the health system. All without adding any additional specialist capacity.