Inpatient Navigation Program
Inpatient Post-Discharge Navigation Program Overview
This presentation provides an overview of Care Continuity's Inpatient Post-Discharge Navigation program. We highlight the challenges with reducing readmissions and explain how health systems can work smarter to prioritize patient outreach to get ahead of common risk factors. With Care Continuity, you can better align your patient navigation and care transition teams to focus on the core drivers of readmissions and ensure that patients comply with follow-up care plans after a recent hospital discharge.
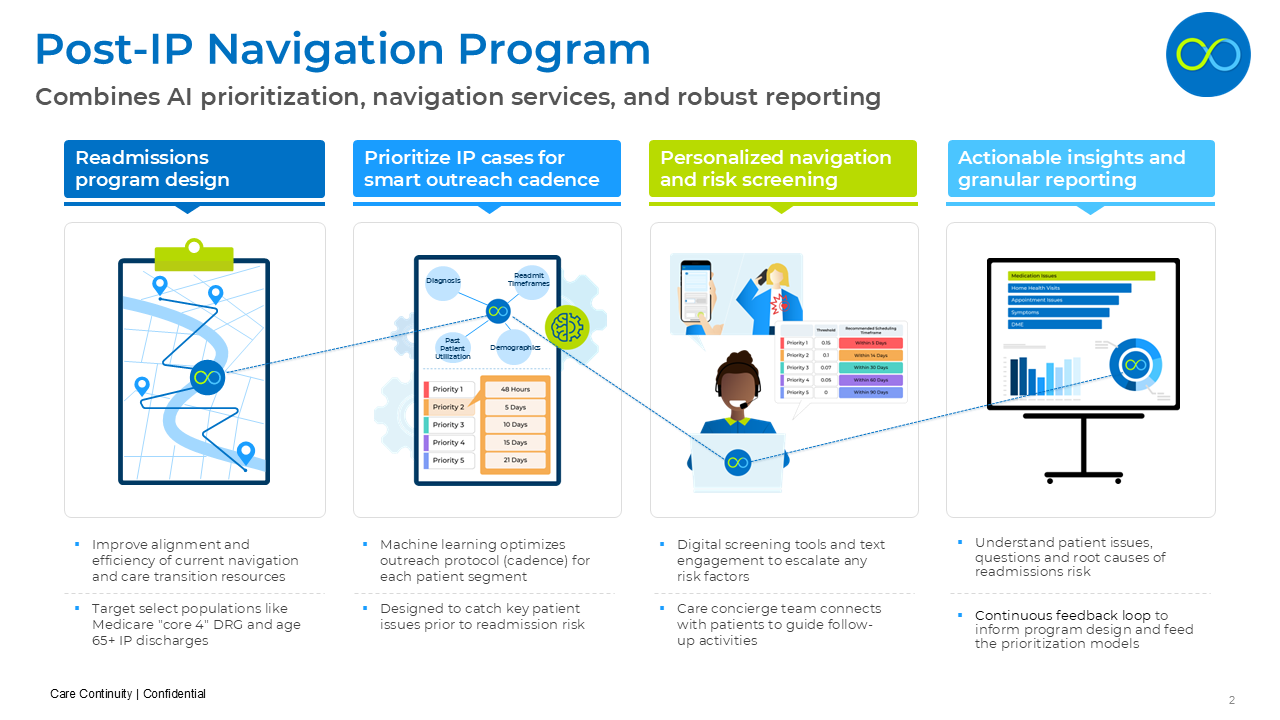
Care Continuity Solution Framework
The Care Continuity Inpatient Navigation program combines AI prioritization models with expert navigation services and granular analytics to tackle the challenge of Inpatient Readmissions. We work closely with our health system partners to understand their current care transition team and design a program that layers in Care Continuity services to focus on specific patient populations. Using machine learning models, we better prioritize inpatient discharges and optimize the follow-up protocol and cadence for each risk segment. We outreach to these patients and engage them to understand potential risk factors, and escalate these problematic patients before they end up back in the hospital. Finally we create granular reports to highlight process challenges and opportunities to improve the program.
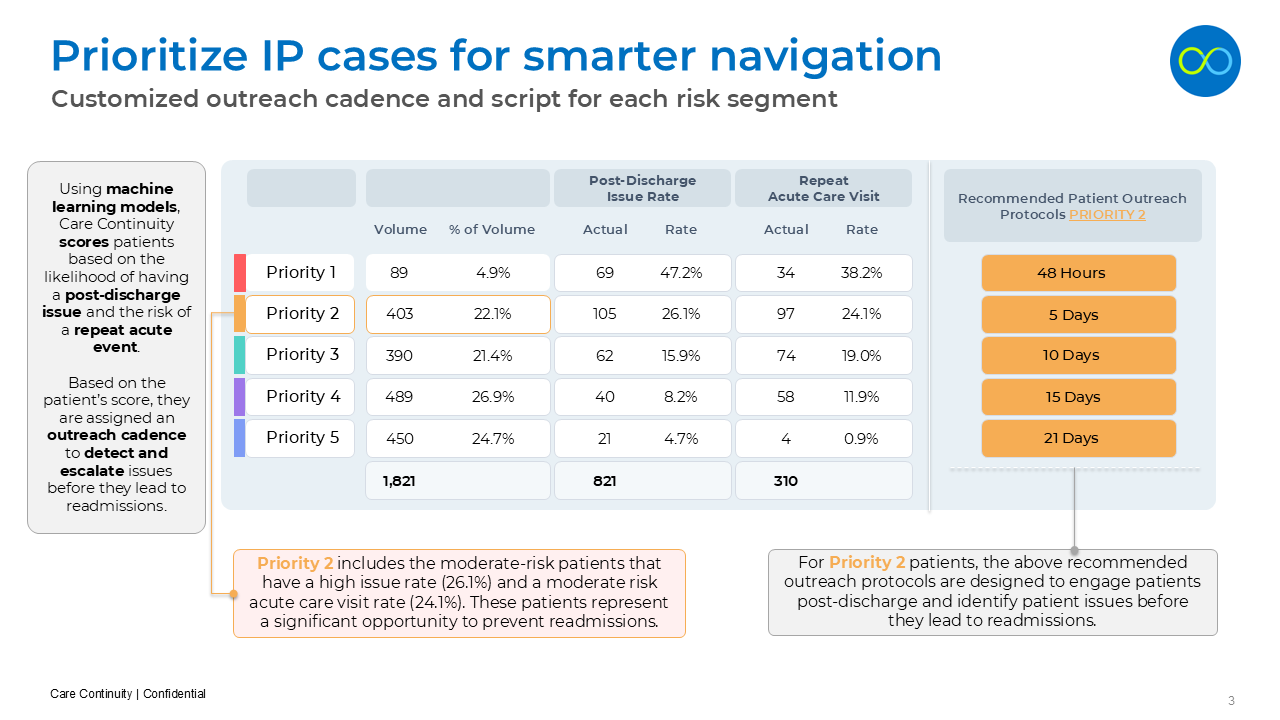
Technology Platform and Segmentation Models
Let's start with how the Care Continuity platform ingests data and uses our predictive models to prioritize patient outreach. We pull in clinical records for every inpatient discharge every day, and create a risk score that stratifies patients based on their likelihood and predicted timing of readmission. We then establish a follow-up protocol for each patient segment, with a different cadence or timeline for outreach and engagement. For certain DRGs and risk profiles we may contact the patient at 48 hours, 3 days and 10 days, while for another segment the cadence might be 72 hours, 5 days and 7 days. Rather than take a one-size-fits-all approach to navigation, the Care Continuity solution relies on a customized outreach timeline for each patient.
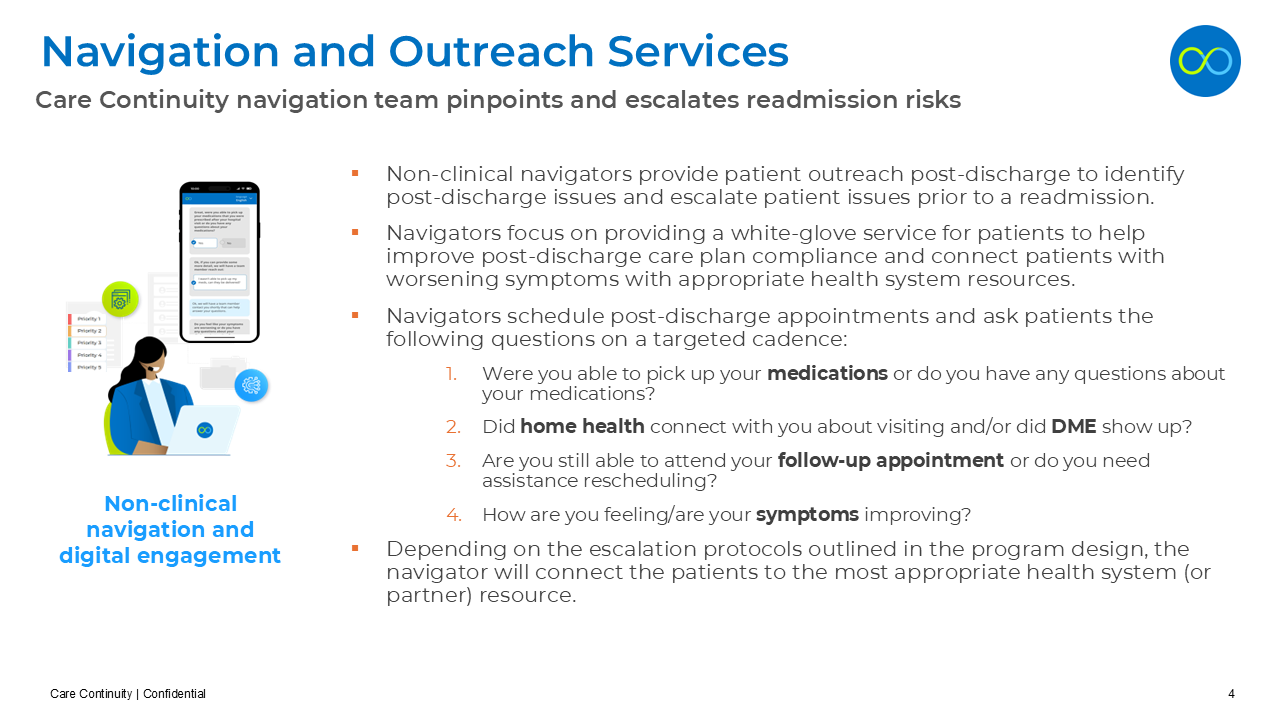
Patient Outreach and Navigation Services
In addition to our technology platform, the Care Continuity program also includes expert navigation staff to communicate with patients, schedule follow-up appointments, and monitor readmission risk factors. Our team of non-clinical concierges provides a white-glove service for key patient populations to improve post-discharge care plan compliance. This team focuses on 5 key questions related to readmission risk - including medication adherence, home health follow-up, DME concerns, follow-up appointments, and worsening symptoms. Based on this patient-reported information, the Care Continuity navigators escalate potential issues before they result in a return inpatient visit.
Virtual Screener and Digital Engagement
The Care Continuity team also uses digital tools to connect with patients and gather readmission risk concerns. We can send a text-based screener to collect information virtually, in a way that is more convenient for some patients. The content of this digital screener is tailored for each patient, and the information gathered is used for immediate escalation and prioritization of intervention strategies.
Example Inpatient Follow-up Workflow
Here's an example of how the Care Continuity Inpatient Navigation Program fits together. First, we focus on a specific inpatient discharge population - in this case Medicare inpatient discharges over age 65with a DRG including heart failure, COPD, pneumonia and AMI. Based on each patient's predicted readmission risk score, we stratify this population and apply a customized outreach cadence for each risk segment. The Care Continuity team engages these patients using a virtual screener and phone outreach to gather readmission risk factors and barriers that might be impacting the post-discharge care plan. This team of navigators then escalates the high-risk patients and collaborates with the health system care team to intervene as necessary.
Granular Analytics and Readmission Root-Cause Analysis
Finally, Care Continuity delivers robust analytics to continually improve the program and adjust the follow-up protocols. We deliver granular reporting for each patient segment and DRG, and track the specific risk factors and barriers that correlate with readmission. In the example here, patients with CHF that indicated issues at 5 days had a readmission rate of17.3% and a median time to readmission of 8.2 days. With the high number of medication issues reported in the first 5 days from discharge, the health system updated their protocol for this segment specifically to boost medication education at the time of discharge. This is one example of how more granular data insights enable a much more detailed understanding of the drivers of readmission risk - and set up a program to intervene with key patients that will truly impact readmission rates.
In Summary
Rather than taking a one-size-fits-all approach to inpatient discharge follow-up, the Care Continuity program supports a smarter approach to prioritizing patient outreach and understanding the drivers of readmission risk. I hope you enjoyed this brief overview. Please download the slides and get in touch with the Care Continuity team if you have any questions.